Reading Duration: 5 minutes
The urinary tract includes the bladder (cystitis), urethra (urethritis, or “wee pipe”), or kidneys (pyelonephritis, kidney infection). UTIs may or may not require treatment, with antibiotics being a potential solution.
To learn more about urinary tract infections (UTI), check this post by the NHS.
Understanding UTI Symptoms
Recognising Common UTI Symptoms
UTI symptoms include:
- A burning or painful sensation during urination (dysuria)
- Increased need to urinate, including at night (nocturia)
- Darker, cloudier, and strong-smelling urine
- High temperature leading to chills or shivering
- Blood in urine
- Aching lower abdomen or back pain
Seeking Medical Attention
When to Consult a GP for UTIs
The NHS advises seeking a GP’s guidance if:
- Experiencing UTI symptoms for the first time
- A child has UTI symptoms
- UTI symptoms occur in men
- Pregnant individuals exhibit UTI symptoms
- Caring for an older person displaying UTI symptoms
- Post-surgery UTI symptoms arise
- Symptoms worsen or don’t improve within 2 days, or return after treatment
Urgent Advice:
When Urgent Attention is Necessary
For urgent assistance, contact a GP or NHS 111 if UTI symptoms, along with specific conditions, manifest, such as:
- Very high or very low temperature
- Confusion or drowsiness
- Pain in the lower abdomen or back, beneath the ribs
- Presence of blood in urine
These indicators could suggest a kidney infection, which requires timely treatment to prevent complications.
Treatment and Self-Care
GP Treatment and Self-Care for UTIs
A GP might perform a urine test to diagnose a UTI. They may:
- Suggest self-care and recommend pain relief
- Prescribe a short antibiotic course
- Prescribe antibiotics while suggesting a 48-hour observation period for symptom improvement
Taking prescribed medicine fully, even if feeling better, is essential.
Managing Recurrent UTIs
Addressing UTIs That Recur
For recurrent UTIs or those appearing twice in 6 months, a GP may:
- Prescribe different or low-dose antibiotics
- Recommend vaginal creams with estrogen (menopausal individuals)
- Refer to specialists for further assessments and treatments
For cases where antibiotics are ineffective or tests miss an infection, a specialist referral might help.
Preventive Measures
Tips for UTI Prevention
To ease UTI symptoms and prevent recurrence:
- Take paracetamol for pain and fever
- Get adequate rest and hydration
- Avoid sexual activity
- Practice good hygiene
- Seek pharmacist assistance
- Follow hygiene tips
Causes and Prevention
Causes and Prevention of UTIs
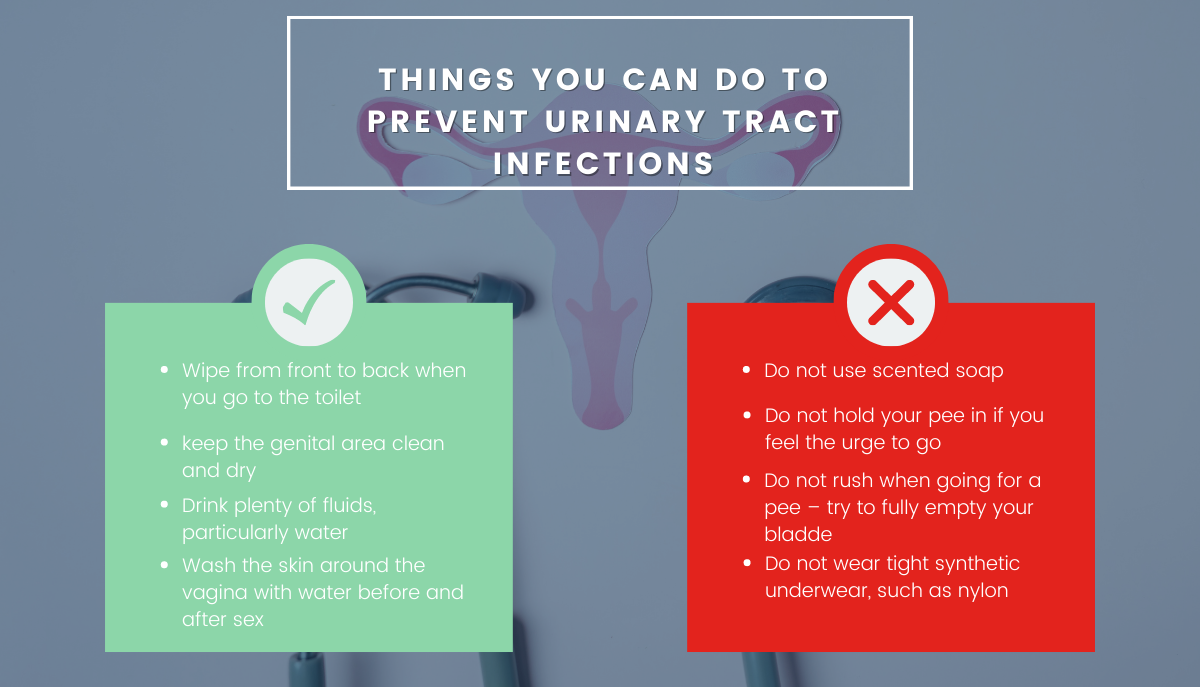
UTIs often stem from bacteria entering the urinary tract through improper hygiene or conditions. Preventive measures include:
- Wiping front to back
- Staying clean and dry
- Staying hydrated
- Hygiene before and after sex
UTIs and Menopause: A Complex Relationship
Hormonal Shifts: During menopause, hormonal changes, specifically a decline in oestrogen levels, can impact the urinary tract’s health. Oestrogen helps maintain the integrity of the urethra and bladder lining, making its reduction a potential risk factor for UTIs.
Vaginal Microbiome: The vaginal microbiome, influenced by hormonal changes, plays a role in UTI susceptibility. A disrupted microbiome balance can lead to changes in vaginal pH, creating an environment conducive to bacterial growth.
Bladder Changes: Menopause-related bladder changes, such as reduced bladder elasticity and weakened pelvic floor muscles, can contribute to incomplete bladder emptying and stagnant urine, fostering UTI development.
Prevention Strategies: Empowering Urological Health
1. Hydration: Staying hydrated helps flush out bacteria and prevent their accumulation in the urinary tract.
2. Personal Hygiene: Proper hygiene, including wiping from front to back after using the toilet, minimises the risk of bacterial transfer.
3. Cranberry Products: Consuming cranberry products or supplements may help prevent bacterial adherence to the urinary tract walls.
4. Oestrogen Therapy: For postmenopausal women, oestrogen therapy, under medical guidance, can help maintain urinary tract health.
5. Urinate Regularly: Avoid holding urine for extended periods, as it can contribute to bacterial growth.
6. Probiotics: Incorporating probiotics into your diet or routine can support a healthy vaginal microbiome.
Incorporating Advice for a Healthy Well-being
Embrace Preventive Actions
This guide assists in understanding UTIs, their symptoms, and how to seek help from the NHS. Incorporating these practices in daily life can contribute to maintaining a healthy well-being.
Make sure you follow us on our socials.
Learn more about vaginal health in our previous blog post here.
Reviewed by: Dr. Helen Kini, NHS GP from Flourish for Life